Can Morton’s Neuroma Cause Sciatica
Can Morton’s neuroma cause sciatica? This question lingers in the minds of many individuals grappling with the debilitating pain of sciatica. Understanding the potential connection between these two conditions is crucial for effective diagnosis and management.
What is Morton’s Neuroma?
Morton neuroma, also known as interdigital neuroma, is a common foot condition characterized by thickening of the tissue around one of the nerves leading to the toes. This often results in sharp, shooting pain in the ball of the foot, typically between the third and fourth toes.

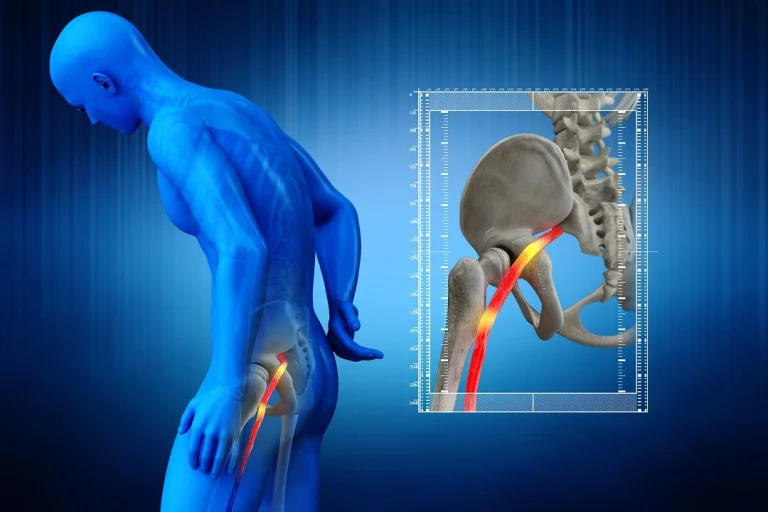
Understanding Sciatica
On the other hand, sciatica refers to pain that radiates along the path of the sciatic nerve, which extends from the lower back through the hips and down each leg. This pain can vary from a mild ache to excruciating discomfort, affecting daily activities and quality of life.
Exploring the Potential Connection
Can Morton’s neuroma cause sciatica? While Morton’s neuroma primarily affects the foot, there is ongoing debate and research regarding its potential to contribute to sciatic nerve irritation. Some studies suggest a possible link, while others propose alternative explanations for sciatic pain.
Scientific Evidence and Statistics
Research published in the Journal of Foot and Ankle Surgery indicates that up to 15% of patients with Morton neuroma also experience symptoms consistent with sciatica. However, it's essential to note that correlation does not imply causation.
A study published in the Journal of Orthopaedic Surgery and Research found that individuals with Morton neuroma were more likely to develop secondary changes in their gait, potentially leading to altered biomechanics and increased pressure on the sciatic nerve.
The Role of Nerve Compression
One possible mechanism linking Morton’s neuroma and sciatica is nerve compression. When the tissue around the foot’s nerves becomes inflamed and enlarged, it can exert pressure on nearby structures, including the sciatic nerve. This compression may contribute to sciatic pain and discomfort.
Differentiating Symptoms
Differentiating between Morton’s neuroma and sciatica symptoms is crucial for accurate diagnosis and treatment. While Morton neuroma typically presents with localized foot pain and numbness, sciatica often involves radiating pain, tingling, and weakness along the leg and into the foot.
Treatment Approaches
Treatment for Morton neuroma and sciatica varies based on the underlying cause and severity of symptoms. For Morton’s neuroma, conservative measures such as orthotic devices, supportive footwear, and corticosteroid injections may provide relief. In more severe cases, surgical intervention may be necessary to remove the affected nerve tissue.
Sciatica management often involves a combination of pain medications, physical therapy, and lifestyle modifications. In some instances, epidural steroid injections or surgical procedures like laminectomy or discectomy may be recommended.
Seeking Professional Guidance
If you’re experiencing symptoms suggestive of Morton neuroma or sciatica, seeking prompt medical evaluation is essential. A healthcare provider can conduct a thorough assessment, including physical examination and diagnostic imaging, to determine the underlying cause of your pain and develop a tailored treatment plan.
Conclusion
Can Morton’s neuroma cause sciatica? While scientific evidence suggests a potential association between these conditions, further research is needed to establish a definitive link. Understanding the mechanisms and distinguishing between their respective symptoms is crucial for accurate diagnosis and effective management.
At Medcareline.com, we strive to provide valuable information and resources for individuals dealing with sciatica and related conditions. Our informational posts cover various aspects of foot health, nerve disorders, and pain management strategies to empower patients in their healthcare journey.
In conclusion, while Morton’s neuroma may contribute to sciatic nerve irritation in some cases, it’s essential to consult with healthcare professionals for personalized assessment and treatment recommendations. Stay informed, stay proactive, and prioritize your well-being.
Frequently Asked Questions
Q1. Can Morton’s neuroma cause numbness and tingling in the legs and feet?
A. While Morton neuroma primarily manifests as localized foot pain and numbness, some individuals may experience referred sensations such as tingling or numbness in the legs and feet. This can occur due to nerve compression and irritation affecting adjacent nerve pathways.
Q2. Are there specific risk factors that increase the likelihood of developing both Morton’s neuroma and sciatica?
A. Certain factors, such as wearing tight or ill-fitting footwear, engaging in repetitive high-impact activities, and having underlying foot deformities, can increase the risk of developing Morton neuroma. Similarly, risk factors for sciatica include age-related changes in the spine, herniated discs, obesity, and occupations requiring prolonged sitting or heavy lifting.
Q3. Can conservative treatments for Morton neuroma also help alleviate sciatica symptoms?
A. While conservative treatments like orthotic devices, supportive footwear, and corticosteroid injections are commonly used for Morton’s neuroma, their effectiveness in addressing sciatica symptoms may vary. However, improving foot biomechanics and reducing nerve irritation in the foot and ankle region can indirectly benefit sciatic nerve function in some cases.
Q4. Is there a connection between Morton’s neuroma and sciatica in pregnancy?
A. Pregnancy-related changes, such as hormonal fluctuations and increased weight-bearing, can contribute to foot issues like Morton’s neuroma. Additionally, the pressure exerted on the spine and pelvic region during pregnancy may exacerbate sciatic nerve compression, leading to sciatica symptoms. Proper footwear, posture support, and gentle exercises can help manage discomfort during pregnancy.
Q5. Can Morton’s neuroma surgery impact sciatica symptoms?
A. Surgical interventions for Morton neuroma, such as nerve excision or decompression procedures, aim to relieve localized foot pain and improve nerve function. While these surgeries target specific foot structures, they may not directly address sciatica symptoms stemming from spinal or nerve root issues. It’s essential to discuss potential outcomes and risks with a healthcare provider before considering surgical options.
Q6. Are there lifestyle modifications that can prevent or alleviate both Morton’s neuroma and sciatica?
A. Maintaining a healthy weight, practicing proper foot care, wearing supportive footwear, and incorporating regular stretching and strengthening exercises can help prevent foot-related conditions like Morton’s neuroma. Similarly, maintaining good posture, avoiding prolonged sitting or standing, and engaging in back-strengthening exercises can reduce the risk of developing or exacerbating sciatica symptoms.
Q7. How can a healthcare provider differentiate between Morton’s neuroma and sciatica during diagnosis?
A. A healthcare provider will typically perform a comprehensive physical examination, including assessing foot biomechanics, evaluating reflexes, and conducting neurological tests, to differentiate between Morton neuroma and sciatica. Diagnostic imaging such as X-rays, ultrasound, or MRI may also be recommended to visualize structural changes and nerve compression patterns.