Can Dehydration Cause Sciatica: Unveiling the Hidden Link
Introduction
Picture this: a warm summer day, and you find yourself immersed in outdoor activities, blissfully unaware that the heat might be conspiring against you. As the temperature rises, so does the risk of dehydration – a seemingly harmless condition with potential repercussions that extend beyond mere thirst. For those grappling with the persistent agony of sciatica, the question arises: Can dehydration cause sciatica?
In this journey through the world of back pain, we’ll unravel the connections between dehydration and sciatica, exploring not only the intricacies of the spine but also how a simple glass of water might hold the key to alleviating your sciatic woes.
A Brief Overview of Sciatica
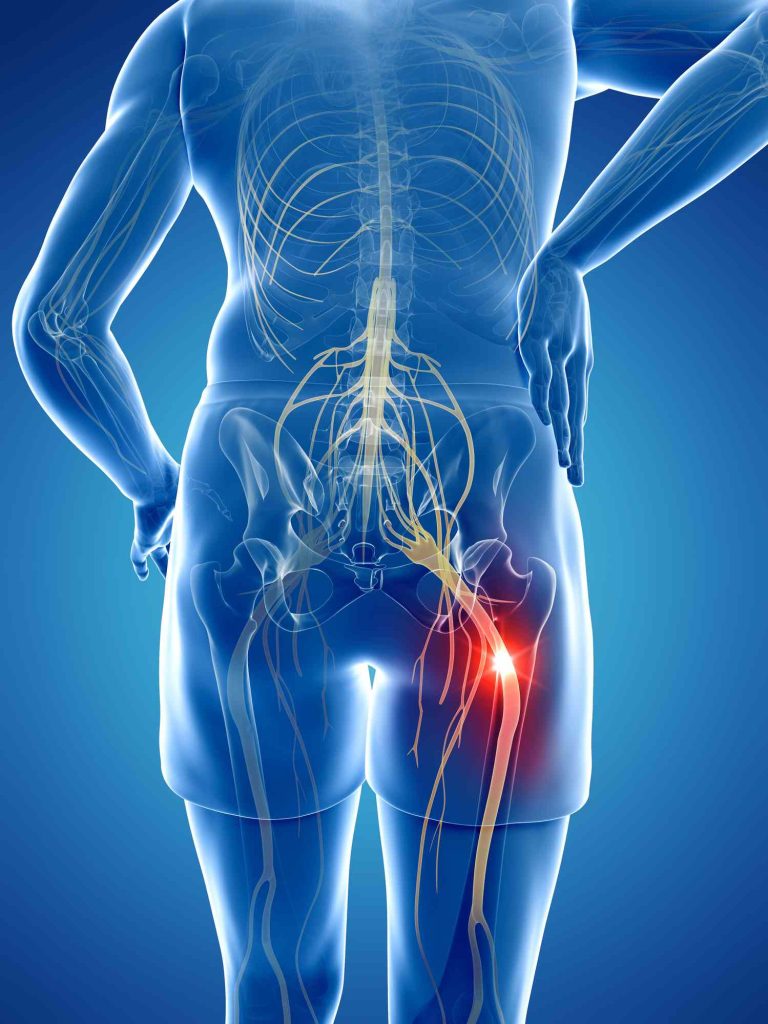
Sciatica, the unwelcome companion on the road of life, manifests as pain radiating along the path of the sciatic nerve – from the lower back through the hips and down each leg. A complex condition often misunderstood, it stems from various underlying issues, including herniated discs, spinal stenosis, and muscle spasms.
Definition & Causes
Diving into the anatomy of sciatica, we discover that it’s not a standalone ailment but rather a symptom of an underlying problem. The interplay between the spinal discs, nerves, and surrounding structures sets the stage for the pain that characterizes sciatica.
Common Symptoms
Sharp, shooting pain, numbness, and tingling sensations – these are the familiar companions of sciatica patients. Recognizing these symptoms is paramount for timely intervention and effective management.
The Connection Between Dehydration and Back Pain, Including Sciatica
The human body, a finely tuned machine, relies on adequate hydration for optimal function. Dehydration can lead to a decrease in the fluid cushioning the spinal discs, resulting in increased friction between the vertebrae. This heightened friction contributes to back pain and, in some cases, exacerbates sciatica symptoms.
Exploring the Intensification of Sciatica Pain in Hotter Seasons

As the temperatures soar, the risk of dehydration amplifies. Understanding the correlation between summertime heat, increased physical activity, and the potential for dehydration sheds light on why sciatica pain might intensify during the warmer months.
Unveiling the Processes in the Spine Amid Back Pain
To truly comprehend the impact of dehydration on sciatica, it’s essential to understand the intricate anatomy of the spine. The spine is a marvel of engineering, composed of vertebrae, intervertebral discs, nerves, and various supporting structures. These components work in harmony to provide flexibility, support, and protection to the spinal cord.
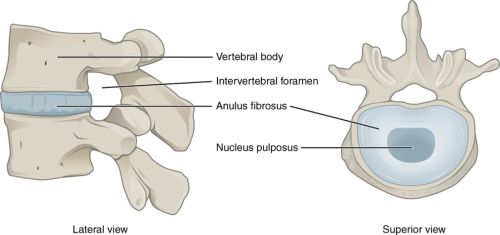
The intervertebral discs, often referred to as the spine’s shock absorbers, play a crucial role. They are gel-like cushions situated between each pair of vertebrae, consisting of a tough outer layer (annulus fibrosus) and a gel-like inner core (nucleus pulposus). These discs not only allow movement between the vertebrae but also act as a buffer, absorbing the stresses and strains endured during daily activities.
The Impact of Dehydration on Spinal Discs
Now, consider the impact of dehydration on these intervertebral discs. Proper hydration is vital for maintaining the discs’ water content. When dehydration occurs, the discs lose their pliability and become less effective in absorbing shocks. The reduction in fluid within the discs can lead to decreased disc height, altering the alignment of the vertebrae and placing additional stress on the spinal structures.
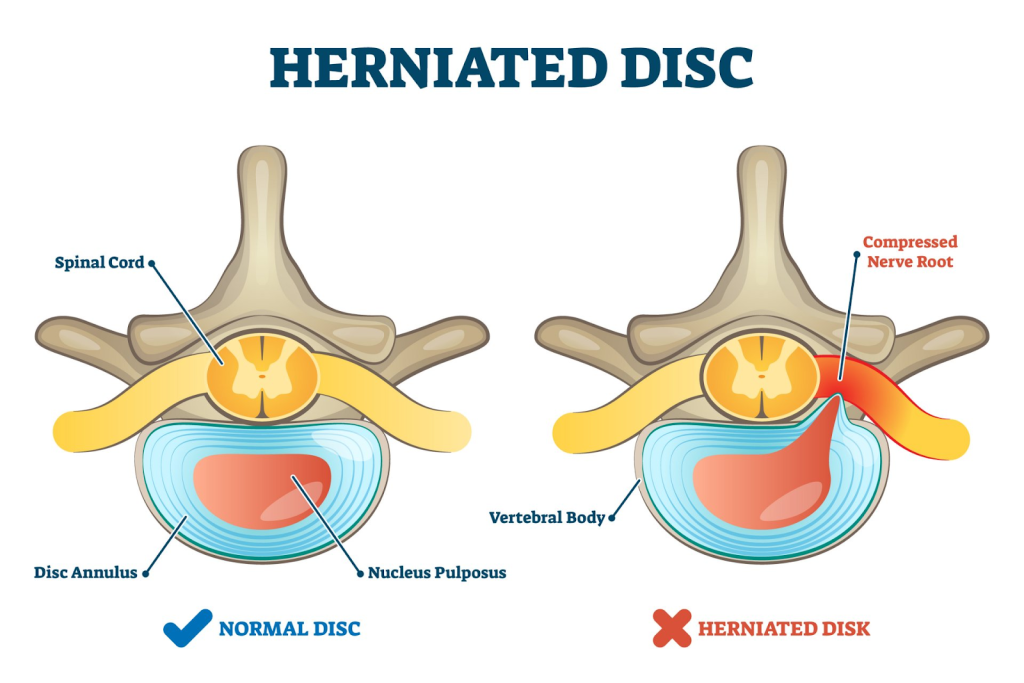
As the discs dehydrate, the annulus fibrosus may become more susceptible to tears or damage, creating an environment conducive to conditions like herniated discs. A dehydrated disc is less able to withstand the compressive forces and may allow the gel-like nucleus pulposus to protrude, potentially impinging on nearby nerves, including the sciatic nerve.
Dehydration’s Role in Fueling Spinal Inflammation
Moreover, dehydration doesn’t solely affect the mechanical aspects of the spine; it also plays a role in inflammation. Dehydrated tissues are more prone to inflammation, and in the context of the spine, this inflammatory response can further irritate the sciatic nerve and exacerbate the pain associated with sciatica.
Inflammation in the spine can contribute to a cascade of events, including the release of inflammatory mediators that sensitize nerve endings and intensify pain signals. The sciatic nerve, already compromised by compression or irritation, becomes more reactive, amplifying the sensations of discomfort and radiating pain.
Understanding these anatomical dynamics reinforces the importance of maintaining adequate hydration for spinal health. Proper fluid intake not only sustains the shock-absorbing capabilities of the intervertebral discs but also mitigates the risk of inflammation and its adverse effects on nerve function.
Signs and Symptoms of Dehydration to Watch For
Understanding the signs of dehydration is crucial. From increased thirst and dark yellow urine to dizziness and fatigue, these indicators serve as warnings that your body needs more fluids.
Recognizing Indicators of Dehydrated Discs
Similarly, recognizing signs of dehydrated discs – such as stiffness, reduced flexibility, and heightened pain during movement – is essential for addressing the root cause of sciatica.
Leveraging Adequate Hydration to Alleviate Pain
The solution may be simpler than you think. Ensuring proper water intake helps maintain spinal disc hydration, reducing friction and easing sciatica symptoms. It’s a fundamental yet often overlooked aspect of sciatica management.
Tips for Maintaining Proper Hydration
Simple habits like carrying a reusable water bottle, setting hydration reminders, and infusing your water with refreshing flavors can make staying hydrated a seamless part of your daily routine.
Beyond Water: Effective Strategies for Optimal Hydration
Hydrating Foods
Include water-rich foods in your diet, such as fruits and vegetables. Watermelon, cucumbers, oranges, and celery are excellent choices. These foods not only contribute to your overall hydration but also provide essential nutrients that support spinal health.
Electrolyte-Rich Beverages
Replenish electrolytes with beverages that go beyond water. Coconut water, sports drinks (low in added sugars), and electrolyte-enhanced water can help maintain the electrolyte balance crucial for proper muscle and nerve function.
Herbal Teas
Opt for caffeine-free herbal teas, such as chamomile or peppermint tea. These not only contribute to your fluid intake but may also have anti-inflammatory properties, potentially aiding in sciatica relief.
Broths and Soups
Incorporate broths and soups into your diet. Not only are they hydrating, but the warm temperature can also be soothing, especially if you’re dealing with inflammation associated with sciatica.
Fruits with High Water Content
Consume fruits with high water content, such as watermelon, strawberries, and cantaloupe. These fruits not only provide hydration but also deliver vitamins and antioxidants that can support overall health.
Hydration Timing
Pay attention to when you hydrate. Drinking water before meals can help with digestion, and having a glass before bedtime can contribute to overall hydration without disrupting sleep with frequent bathroom visits.
Avoid Dehydrating Substances
Limit the consumption of substances that can contribute to dehydration, such as caffeinated and alcoholic beverages. Both can have diuretic effects, leading to increased fluid loss.
Coconut Water
Coconut water is not only a refreshing beverage but also a good source of electrolytes. It can be particularly beneficial for rehydration after physical activity, providing potassium, sodium, and magnesium.
Hydration Through Food Preparation
Consider incorporating water-rich foods into your meals, such as adding sliced cucumbers to salads or having a bowl of watermelon as a snack. This not only enhances flavor but also contributes to your overall hydration.
Incorporate Hydrating Snacks
Choose hydrating snacks like yogurt, which not only provides fluids but also offers calcium and probiotics that can be beneficial for bone and digestive health.
Remember, while these strategies contribute to overall hydration, water remains the primary and most essential hydrating agent. Tailoring your approach to include a variety of hydrating sources can complement your fluid intake and support sciatica relief.
Cultivating Healthy Hydration Practices
Hydration is not a one-size-fits-all solution. Tailoring your hydration habits to your lifestyle and individual needs is crucial for sustained well-being and sciatica management.
Conclusion
As we navigate the intricate terrain of sciatica and its connection to dehydration, one question lingers – can a glass of water truly hold the key to relieving sciatic pain? The answer may be simpler than we realize. In the pursuit of a pain-free existence, let hydration be your ally, quenching not just your thirst but also the flames of sciatica.
In the world of sciatica, where every step can be a challenge, the question remains: How can your hydration choices pave the way for a life unburdened by sciatic pain?
Frequently Asked Questions
Q: Can drinking more water alleviate sciatica pain immediately?A: While proper hydration is essential for spinal health, it may not provide immediate relief. Consistent hydration supports overall well-being and may contribute to long-term sciatica management.
Q: Are certain individuals more prone to dehydration-related sciatica?A: Individuals who engage in strenuous physical activities, especially in hot climates, may be more prone to dehydration which can cause sciatica. Athletes and those with physically demanding jobs should be particularly vigilant about staying hydrated.
Q: Is there a link between dehydration and muscle cramps associated with sciatica?A: Dehydration can contribute to muscle cramps, which can cause sciatica symptoms. Adequate hydration supports muscle function and helps prevent cramping.
Q: Can dehydration affect the effectiveness of sciatica treatments?
A: Dehydration may impact the efficacy of certain treatments for sciatica, such as physical therapy. Proper hydration ensures that the body can respond optimally to therapeutic interventions.
Q: Does dehydration increase the risk of sciatica recurrence?A: Chronic dehydration may contribute to conditions that lead to sciatica, potentially increasing the risk of recurrence. Maintaining proper hydration levels is crucial for long-term spinal health.
Q: Can dehydration-related headaches contribute to sciatica pain?A: Dehydration-related headaches may exacerbate overall discomfort, including sciatica pain. Staying well-hydrated can help manage headaches and contribute to a more comfortable experience for individuals with sciatica.
Q: Are there specific exercises that can worsen sciatica symptoms in a dehydrated state?A: Dehydration can compromise muscle function, potentially making certain exercises more challenging. Staying hydrated ensures that muscles are adequately lubricated and can support movement without exacerbating sciatica symptoms.
Q: Can dehydration affect the response to medications used for sciatica pain?A: Dehydration may influence how the body metabolizes medications. Ensuring proper hydration can contribute to the optimal effectiveness of medications prescribed for sciatica relief.
References
- Rubin, D. I. (2007). Epidemiology and risk factors for spine pain. Neurologic Clinics, 25(2), 353-371. https://pubmed.ncbi.nlm.nih.gov/17445733/
- Deyo, R. A., & Weinstein, J. N. (2001). Low back pain. New England Journal of Medicine, 344(5), 363-370. https://www.nejm.org/doi/full/10.1056/nejm200102013440508
- Blau, J. N. (2004). Water‐deprivation headache: a new headache with two variants. Headache: The Journal of Head and Face Pain, 44(1), 79-83. https://pubmed.ncbi.nlm.nih.gov/14979888/
- Popkin, B. M., D’Anci, K. E., & Rosenberg, I. H. (2010). Water, hydration, and health. Nutrition Reviews, 68(8), 439-458. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2908954/
- Wannamethee, S. G., Lowe, G. D., Rumley, A., Bruckdorfer, K. R., Whincup, P. H., & Walker, M. (2006). Associations of vitamin C status, fruit and vegetable intakes, and markers of inflammation and hemostasis. The American Journal of Clinical Nutrition, 83(3), 567-574. https://pubmed.ncbi.nlm.nih.gov/16522902/
- Adams, M. A., & Roughley, P. J. (2006). What is intervertebral disc degeneration, and what causes it? Spine, 31(18), 2151-2161. https://pubmed.ncbi.nlm.nih.gov/16915105/
- Urban, J. P. G., Smith, S., & Fairbank, J. C. T. (2004). Nutrition of the intervertebral disc. Spine, 29(23), 2700-2709. https://pubmed.ncbi.nlm.nih.gov/15564919/
- Freemont, A. J. (2009). The cellular pathobiology of the degenerate intervertebral disc and discogenic back pain. Rheumatology, 48(1), 5-10. https://pubmed.ncbi.nlm.nih.gov/18854342/