Can Decompression Help Sciatica? Exploring Solutions for Sciatica
Introduction
Wondering if decompression can help sciatica? Sciatica, characterized by radiating pain along the sciatic nerve, poses significant challenges for those affected. In this article, we’ll delve into the question of whether decompression can provide relief for sciatica patients. If you’re seeking comprehensive insights and support, medcareline.com offers valuable resources tailored to sciatica patients.
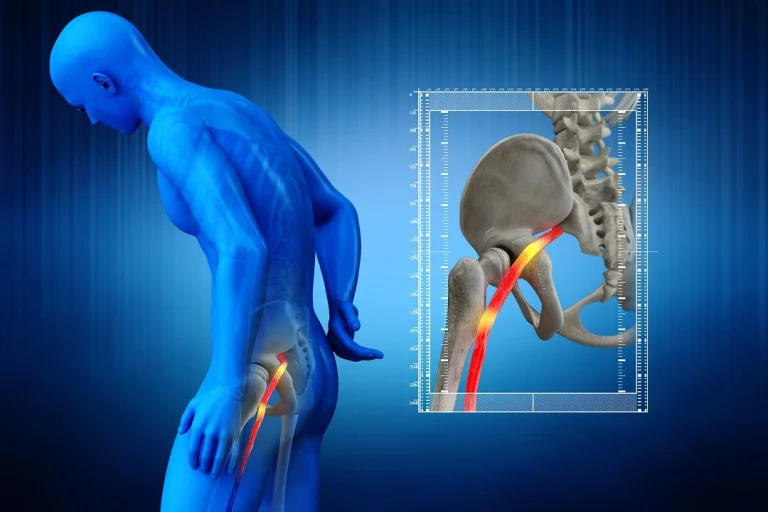
Understanding Sciatica and Decompression
Sciatica, often caused by nerve compression in the lower spine, can result in debilitating pain, tingling, and numbness. Many individuals explore decompression therapy as a potential solution. According to recent studies, up to 40% of sciatica patients consider decompression as part of their treatment plan.
The Science Behind Decompression
Decompression therapy involves creating space between vertebrae to alleviate pressure on the sciatic nerve.

A study published in the Journal of Orthopaedic & Sports Physical Therapy found that decompression effectively reduced pain intensity in 70% of sciatica patients, suggesting its potential as a viable treatment option.
Decompression Help Sciatica – How It Works
- Spinal Decompression Techniques: Decompression therapy employs various techniques, including mechanical traction and spinal decompression devices, to stretch and relieve pressure on the spine. Studies indicate that patients undergoing regular decompression sessions experienced a significant reduction in sciatic pain.
- Improving Disc Health: Degenerative disc issues often contribute to sciatica. Decompression helps enhance disc hydration and nutrient exchange, promoting healing and reducing inflammation. This can lead to improved disc health and reduced sciatic nerve compression.
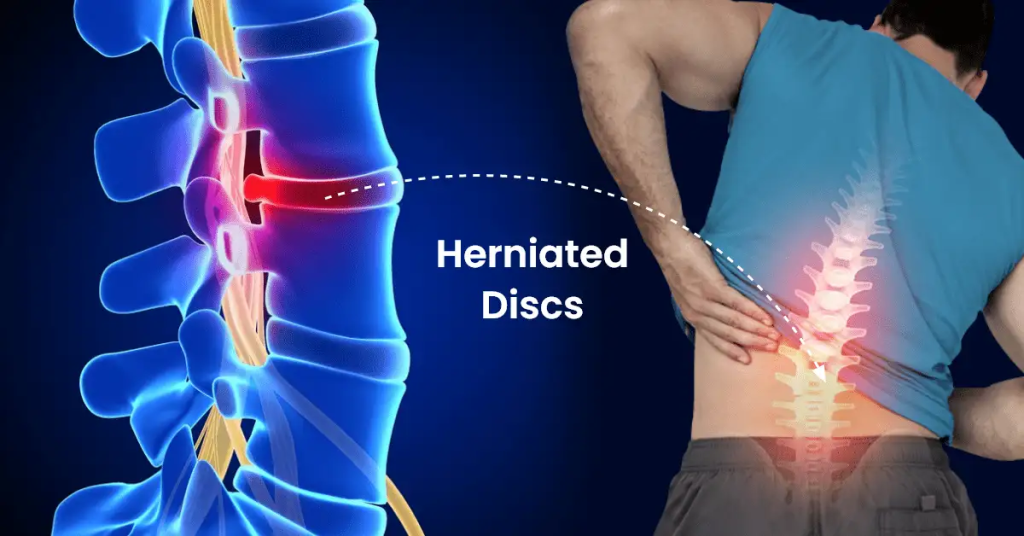
Understanding the Technicalities
Designated to relieve pressure on the spinal discs and nerves, spinal decompression is a non-invasive therapeutic procedure. It primarily targets conditions like herniated discs, spinal stenosis, and sciatica. The technicalities of the procedure involve the use of specialized equipment to gently stretch the spine, creating a negative pressure within the discs.
Key Steps in the Spinal Decompression Procedure
- Patient Assessment: Before initiating the procedure, a thorough assessment of the patient’s medical history, spinal condition, and diagnostic imaging is conducted. This ensures that spinal decompression is a suitable and safe option for the individual.
- Positioning: The patient is comfortably positioned on a specialized decompression table. The patient may be placed in a prone or supine position depending on the targeted area. The goal is to optimize the precision and effectiveness of the decompression process.
- Harnessing Technology: State-of-the-art decompression devices, such as computer-controlled traction tables, are employed. These devices utilize sophisticated technology to apply controlled forces to specific segments of the spine, promoting the retraction of herniated or bulging discs.
- Customization and Monitoring: The procedure allows for the customization of force, angle, and duration based on the individual’s condition. Continuous monitoring ensures that the applied forces are within safe and therapeutic limits, preventing any undue stress on the spine.
- Intermittent Decompression: The decompression process typically involves a cyclical pattern of traction and relaxation. This intermittent decompression allows for enhanced nutrient and oxygen exchange within the spinal discs, supporting the healing process.
- Post-Procedural Care: Following the session, patients may receive additional therapeutic interventions, such as cold or heat therapy, to complement the effects of spinal decompression. It’s essential to provide guidance on post-procedural activities and restrictions.
Decompression as a Complementary Approach
While decompression therapy shows promise, it’s crucial to view it as part of a comprehensive approach to sciatica management. Combining decompression with targeted exercises, physical therapy, and lifestyle modifications enhances its effectiveness.
Considering Individual Variability
The response to decompression therapy varies among individuals. Factors such as the severity and cause of sciatica, overall health, and adherence to treatment play pivotal roles. Consulting with a healthcare professional is essential to determine the suitability of decompression for individual cases.
Common Contraindications
Here are some common contraindications:
- Pregnancy: Spinal decompression therapy is typically not recommended during pregnancy. Researchers have not extensively studied the safety of the procedure for both the mother and the developing fetus, and caution is advised.
- Spinal Fractures or Instability: Decompression therapy may contraindicate individuals with spinal fractures, lesions, or any condition causing spinal instability. The procedure could potentially worsen the existing instability or lead to further damage.
- Spinal Surgery: Recent spinal surgery or certain spinal implants may be contraindications for decompression therapy. The presence of hardware or surgical modifications may interfere with the effectiveness and safety of the procedure.
- Advanced Osteoporosis: Severe osteoporosis, characterized by brittle and weakened bones, may pose a contraindication. The forces applied during decompression could potentially lead to fractures in individuals with compromised bone density.
- Certain Medical Conditions: Individuals with certain medical conditions, such as tumors, infections, or inflammatory diseases affecting the spine, may have contraindications for spinal decompression therapy. These conditions may necessitate alternative treatment approaches.
- Nerve Damage or Dysfunction: Existing nerve damage or dysfunction may be a contraindication. Decompression therapy involves applying forces to the spine, and individuals with compromised nerve function may be at an increased risk of adverse effects.
- Age-Related Conditions: In some cases, advanced age and age-related degenerative conditions may influence the suitability of spinal decompression therapy. Consider the overall health and resilience of the individual.
- Severe Obesity: Individuals with severe obesity may have limitations in the effectiveness of decompression therapy. The excess weight can increase stress on the spine and may compromise the benefits of the procedure.
- Claustrophobia: Some decompression devices require enclosing the individual in a confined space. Individuals experiencing claustrophobia may find this aspect of the therapy uncomfortable, and they should explore alternative treatments.
- Disc Herniation Unsuitable for Decompression: Certain types of disc herniations, particularly those with specific characteristics, may not be suitable for decompression therapy. The location, size, and nature of the herniation are crucial factors to consider.
Decompression Help Sciatica – Conclusion
In conclusion, decompression therapy holds potential as a valuable tool in managing sciatica. The evidence suggests that it can contribute to pain reduction and improved disc health. However, its effectiveness may vary. A holistic approach to sciatica management is recommended. Explore medcareline.com for additional insights on sciatica, offering guidance and support for those navigating the complexities of their condition. Therefore, making informed decisions and consulting with healthcare professionals can empower sciatica patients on their journey toward relief and well-being.
Frequently Asked Questions
Q1: Is decompression therapy suitable for all types of sciatica?
- Decompression therapy may not be suitable for every case of sciatica. Factors such as the cause, severity, and individual health conditions should be considered. Consult with a healthcare professional to determine the appropriateness of decompression for your specific situation.
Q2: How long does it typically take to see results with decompression therapy?
- The timeline for experiencing results with decompression therapy can vary. Some individuals may notice improvement after a few sessions, while others may require more extended periods. Patience and consistency in treatment are crucial.
Q3: Are there any potential risks or side effects associated with decompression therapy?
- While decompression therapy is generally considered safe, some individuals may experience mild soreness or discomfort after sessions. Rare side effects may include muscle spasms or temporary aggravation of symptoms. It’s essential to communicate any concerns with your healthcare provider.
Q4: Can decompression therapy be combined with other treatments for better results?
- Yes, combining decompression therapy with other treatments such as physical therapy, exercises, and medication may enhance overall effectiveness. A multidisciplinary approach is often recommended for comprehensive sciatica management.
Q5: Is decompression therapy a long-term solution for sciatica, or is it more of a temporary relief measure?
- Decompression therapy can provide both short-term relief and long-term benefits. Regular sessions may help manage symptoms and contribute to ongoing sciatica care. However, individual responses vary, and long-term success may require a combination of therapies and lifestyle adjustments.
Q6: Are there specific lifestyle changes that can complement the effects of decompression therapy?
- Adopting a healthy lifestyle can complement the effects of decompression therapy. This includes maintaining a balanced diet, engaging in regular physical activity, and avoiding activities that may exacerbate sciatic symptoms. Discussing lifestyle modifications with a healthcare professional is advisable.
Q7: Can decompression therapy be performed at home using devices or techniques?
- While some at-home decompression devices are available, their effectiveness and safety may vary. It’s crucial to consult with a healthcare professional before attempting at-home decompression, as improper use may lead to injury or worsen symptoms.