Sciatica Trigger Points Map: A Comprehensive Guide
Introduction
Sciatica affects millions of people worldwide and causes pain, discomfort, and limited mobility. Among the myriad factors that cause sciatica, trigger points play an important role. Tension and tenderness in these localized muscles can significantly worsen sciatica symptoms. Understanding the sciatica trigger points map is critical to effectively treating and relieving this debilitating condition.
This comprehensive guide explores the science behind trigger points, explores common trigger points associated with sciatica, discusses strategies for relief, and discusses various types of pain, including axial sciatica and appendicular sciatica. Learn about the different sciatica types, how to test for sciatica, and address frequently asked questions.
The Science Behind Trigger Points
Trigger Point Definition
Trigger points are areas prone to overstimulation located in tense ligaments of skeletal muscles. Pressing these pressure points will not only cause you to feel pain, but it can also spread the pain to other parts of your body. Pain caused by trigger points can mimic sciatica symptoms, making it necessary to identify and target these specific areas.
Mechanisms of Trigger Points Causing Sciatica
When trigger points form in the muscles connected to the sciatic nerve, they can cause or worsen sciatica through a variety of mechanisms. A common scenario is compression of the sciatic nerve by tight or inflamed muscles. For example, if you have a trigger point in your piriformis muscle, it can compress your sciatic nerve and cause referred pain in your leg.
Additionally, trigger points can cause a phenomenon known as “referred pain.” This occurs when the pain is felt in an area distant from the trigger point itself. In sciatica, trigger points in muscles such as the piriformis and gluteus medius can transmit pain down the legs, mimicking the symptoms of true sciatica.
Common Trigger Points for Sciatica
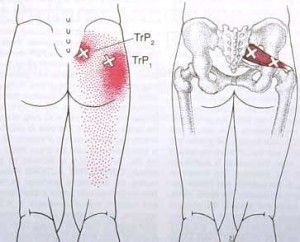
- Piriformis Muscle: The piriformis muscle, located in the buttocks, is a common trigger point for sciatica. When this muscle becomes tight or trigger points develop, it can compress the sciatic nerve and cause referred pain in the leg. Symptoms can be relieved with techniques such as self-massage and stretching exercises that are specific to the piriformis muscle.
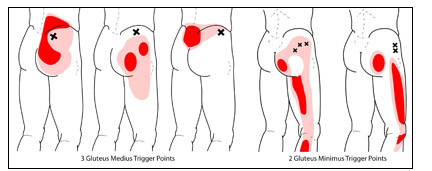
- Gluteus medius and minimus: These muscles play an important role in stabilizing the pelvis and are often involved in sciatica pain. Trigger points in the gluteus medius and medius muscles can cause pain in the lower back and legs. Incorporating stretches and massage techniques that target these muscles can help relieve pain and improve overall mobility.
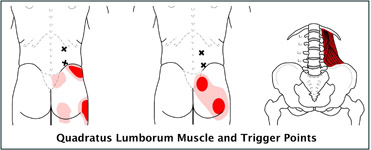
- Quadratus Lumborum Muscle: The quadratus lumborum muscle is located in the lower back and can contribute to the development of sciatica when trigger points occur. Tension in this muscle can cause pain that radiates down your butt and thighs. Proactive measures such as stretching and strengthening exercises can prevent or alleviate trigger points in the quadratus lumborum muscle.
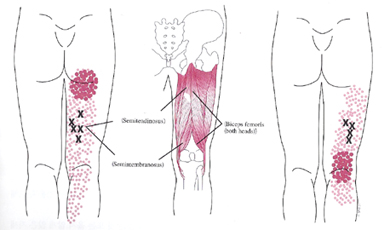
- Hamstrings: Tightness of the thigh muscles is a common problem and the presence of trigger points can lead to sciatica. Regular stretching and strengthening exercises for the hamstring muscles can help relieve tension and reduce symptoms.
- Iliopsoas: The iliopsoas consist of the psoas major and iliac muscles and is located deep in the abdominal cavity. Trigger points in this muscle can transmit pain to your lower back, causing sciatica symptoms. Stretching and massage techniques that target the iliopsoas muscle can help treat sciatica.
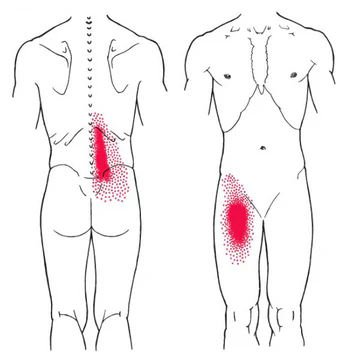
Sciatica Trigger Points Map: Visual Guide
Imagine your body as an interconnected network of muscles. Certain trigger points act as potential sources of pain. Visualizing a map of sciatica trigger points can help you understand the relationship between trigger points and sciatica pain. This map serves as a valuable tool for identifying and treating trigger points associated with sciatica.
Types of Sciatica
Axial Sciatica
Axial sciatica refers to pain that radiates along the path of the sciatic nerve. Usually, it runs from the lower back through the buttocks and down the back of the legs. This type of sciatica often results from compression of nerve roots in the lumbar spine and is often caused by conditions such as herniated discs or spinal stenosis.
Appendicular Sciatica
Appendicular Sciatica, on the other hand, is characterized by pain that radiates down the leg but does not necessarily follow the path of the sciatic nerve. This type of sciatica can be caused by trigger points, muscle imbalances, or other factors not related to the disc. Identifying the specific type of sciatica is critical to implementing targeted treatment strategies.
How to Test for Sciatica
Diagnosing sciatica often requires a combination of medical history, physical examination, and imaging tests. Common testing methods include:
- Physical Exam: A thorough physical exam by your doctor can help identify the signs and symptoms of sciatica. This may include evaluating muscle strength, reflexes, and sensation in the affected leg.
- Straight Leg Raise Test: The Straight Leg Raise Test involves lifting your leg while lying down to see if and how much pain occurs. This test can indicate inflammation of the nerve roots, which is a common cause of sciatica.
- Imaging studies: X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) provide detailed images of the spine to detect herniated discs, spinal stenosis, or other symptoms that can lead to sciatica.
- Electromyography (EMG): EMG measures electrical activity in muscles and helps determine if there is nerve damage or compression that contributes to sciatica symptoms.
- Nerve Conduction Studies: These studies assess how well the sciatic nerve conducts electrical impulses and help identify areas of nerve compression or damage.
Strategies for Relief
- Self-Massage Techniques: Learning self-massage techniques can empower people suffering from sciatica. Using a tool like a foam roller or tennis ball to apply gentle pressure to the trigger points in the affected muscles can relieve tension and reduce pain.
- Stretching Exercises: Incorporating targeted stretching exercises into your daily routine can improve flexibility and reduce muscle tension. Focus on stretching exercises that specifically target the muscles associated with sciatica trigger points, such as Piriformis, hamstrings, and hip flexors.
- Hot and Cold Therapy: Alternating hot and cold therapy is effective in treating sciatica pain. Heat therapy relaxes tense muscles, and cold therapy reduces inflammation. Experiment with heat packs and ice packs to find the combination that works best for you.
- Physical Therapy: Seek advice from a physical therapist for personalized strategies for treating sciatica. A therapist can assess your specific trigger points and design a targeted exercise and stretching program tailored to your individual needs.
- Mind-Body Techniques: Stress and tension can worsen sciatica pain. Mind-body techniques such as yoga, meditation, and breathing exercises can help manage stress, promote relaxation, and reduce overall pain.
Frequently Asked Questions
Q1: Can trigger points themselves cause sciatica?
Yes, trigger points in certain muscles can contribute to or cause sciatica-like symptoms. For example, if you have a trigger point in your piriformis muscle, it can compress your sciatic nerve and cause referred pain in your leg.
Q2: How can I massage trigger points myself at home?
You can use tools such as a foam roller or tennis ball to apply gentle pressure to trigger points. Roll or press on the affected muscles, focusing on areas of tenderness or stiffness. Remember to start with light pressure and gradually increase the pressure as per your tolerance.
Q3: Are there any special exercises to prevent the formation of trigger points?
Yes, incorporating stretching and strengthening exercises into your daily routine can help prevent trigger points. Focus on exercises that target muscles that tend to get tight, hamstrings, piriformis, and hip flexors.
Q4: What lifestyle changes can help treat sciatica symptoms?
Good posture, regular exercise, and avoiding prolonged sitting can help reduce sciatica symptoms. Additionally, practicing stress reduction techniques such as yoga and meditation can be helpful.
Q5: How long does it take to see improvement with trigger point therapy?
The timeline for improvement varies from person to person. Consistency is key, and individual patients may experience symptom relief within a few weeks of regular trigger point therapy. However, it’s important to stick with these habits for long-term benefits.
Conclusion
Understanding the sciatica trigger points map is an important step to relief and recovery. Recognizing and treating trigger points through techniques such as self-massage, stretching, and therapeutic exercise can help you proactively manage your sciatica pain. Recognizing different types of sciatica, such as axial sciatica and appendicular sciatica as described above, allows for a more differentiated treatment approach.
Incorporating testing methods helps in accurate diagnosis and guides healthcare professionals to effective interventions. Consistency is key and we recommend consulting your health care professional for personalized advice and treatment options. With the right approach, individuals can find relief from symptoms and control over their mobility and health. This journey to pain relief is not only about understanding trigger points but also about taking active steps toward a pain-free life.
References
- Qianjun Jin, Yuxin Chang, Chenmiao Lu, Lunhao Chen, Yue Wang. (2023). Referred pain: characteristics, possible mechanisms, and clinical management. Frontiers in Neurology. 14. https://doi.org/10.3389/fneur.2023.1104817
- Travell, J., & Simons, D. (1992). Myofascial pain and dysfunction: the trigger point manual. Volume 1, Upper half of body. Lippincott Williams & Wilkins.
- Nee, R. J., & Butler, D. S. (2006). Management of peripheral neuropathic pain: Integrating neurobiology, neurodynamics, and clinical evidence. Physical Therapy in Sport, 7(1), 36-49.
- Simons, D. G., Travell, J. G., & Simons, L. S. (1999). Travell & Simons’ Myofascial pain and dysfunction: The trigger point manual (Vol. 2, The lower extremities). Lippincott Williams & Wilkins.
- Maigne, J. Y., Doursounian, L., & Chatellier, G. (1996). Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma. Spine, 21(22), 2588-2592.








I am genuinely amazed with your deep insights and excellent ability to convey information. Your expertise shines through in every sentence. It’s obvious that you spend considerable time into researching your topics, and that effort does not go unnoticed. We appreciate your efforts in sharing such valuable insights. Keep up the great work! https://rochellemaize.com
I’m thoroughly captivated by the deep insights and excellent way of expressing complex ideas. The knowledge you share clearly stands out in each paragraph. It’s obvious that you spend considerable time into understanding your topics, and that effort does not go unnoticed. Thank you for sharing such valuable insights. Keep on enlightening us! https://www.elevenviral.com