What is Stage 4 Sciatica ?
Introduction
Stage 4 sciatica can be described as severe chronic sciatica, but this term is not recognized. There is generally no accepted staging system specific to sciatica. Unlike some medical conditions, such as cancer, which have well-defined stages, sciatica is generally characterized by acute or chronic duration, underlying cause, and severity of symptoms (mild, moderate, or severe).
Let’s break down sciatica into simpler terms, explore its different aspects, and find out how to deal with this common but often misunderstood condition.
Sciatica Overview
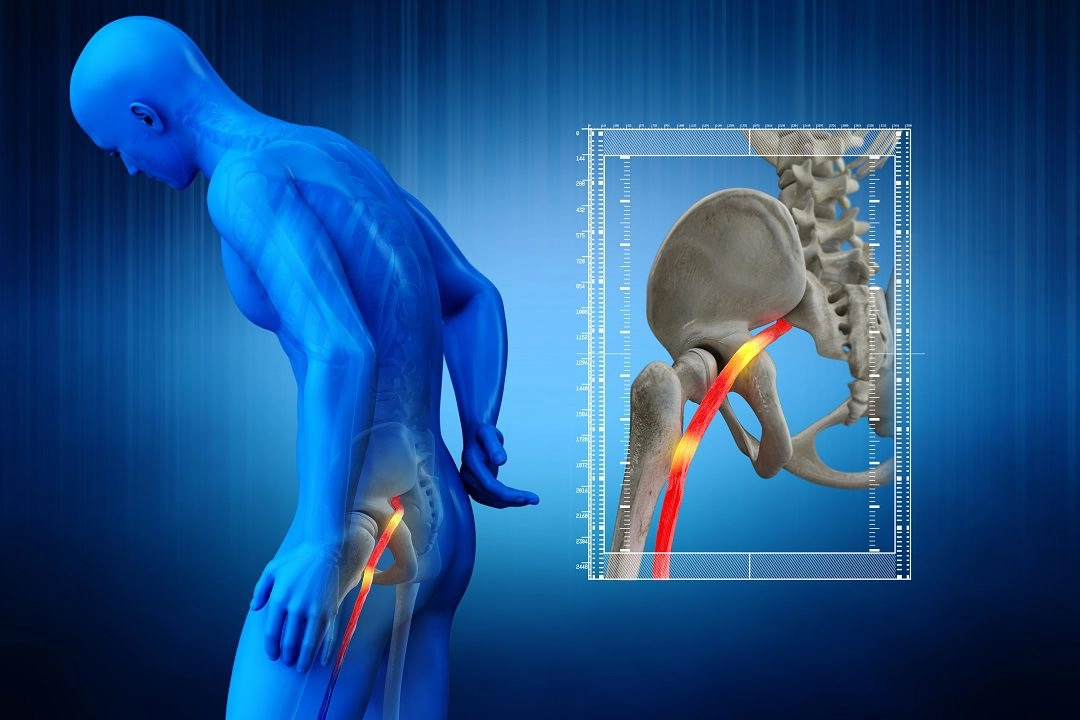
Imagine your spine as a complex highway, with the sciatic nerve being the main route running from your lower back to each leg.
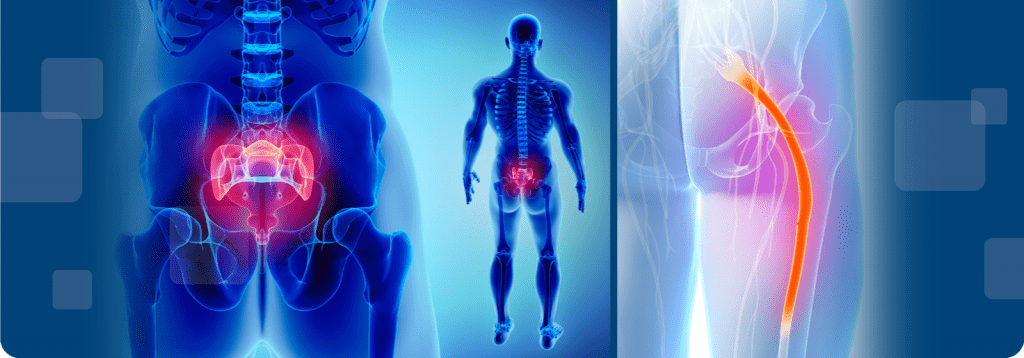
When this nerve becomes irritated or compressed, it causes a series of symptoms collectively known as sciatica. These symptoms include pain, tingling, and sometimes weakness in the lower back, buttocks, and legs.
Understanding Duration: Acute vs.Chronic Sciatica
Sciatica can be classified based on its duration:
1. Acute Sciatica: This type of sciatica occurs suddenly and is often accompanied by certain phenomena, such as a herniated disc.
Symptom: severe stabbing pain that requires immediate attention.
Outlook: Acute sciatica symptoms usually respond well to immediate treatment.
2. Chronic Sciatica (stage 4 sciatica): Pain is considered chronic if it lasts for more than three months and may be related to an ongoing problem, such as aging or persistent back problems.
Symptoms: long-term symptoms that require a more comprehensive approach.
Perspectives: Treatment of chronic sciatica requires a more comprehensive and integrated strategy.
Identifying the Culprit: Common Causes of Sciatica
To understand sciatica, you need to understand what is causing the discomfort.
Common causes include:
1. Slipped Disc: The soft material of the discs in the spine can protrude and irritate nearby nerves.
Effect: sharp stabbing pain in the leg.
2. Spinal stenosis: Narrowing of the spinal canal, putting pressure on the spinal cord and nerves.
Effects: Pain worsens when standing or walking.
3. Degenerative Disc Disease: Wear of the intervertebral discs that occurs as part of the aging process.
Impact: chronic pain due to intervertebral disc degeneration.
4. Piriformis Syndrome: Compression of the sciatic nerve by the piriformis muscle of the buttock.
Effects: pain, tingling, or numbness along the sciatic nerve pathway. Intensity Rating: Mild to Severe Sciatica
Understanding the Severity of Sciatica
Understanding the severity of sciatica can help characterize the intensity of your symptoms.
1. Mild sciatica: There is occasional discomfort and dull pain, and activities of daily living are significantly impaired.
2. Moderate sciatica: A noticeable symptom that occurs more frequently. You may need to make adjustments to your daily routine.
3. Severe sciatica (stage 4 sciatica): Excruciating pain that seriously interferes with daily life and may require more aggressive treatment.
Decoding Nerve Signals
Sciatica is often accompanied by specific signals indicating nerve involvement:
1. Numbness: A sensation of decreased or no sensation in the affected area. Meaning: Indicates compression or irritation of a nerve.
- Tingling: “Pins and needles” sensation.
Meaning: Pain often precedes or is accompanied by additional information about the condition of the nerve. - Muscle Weakness: Difficulty lifting the leg or moving the affected leg.
Meaning: Indicates significant nerve compression that affects muscle control. - Reflex changes: Reflex test responses have been changed.
Meaning: Indicates a neurological problem that requires further investigation.
Diagnosis and Treatment of Sciatica
Determining the cause of sciatica requires a professional diagnosis and targeted treatment.
- Examination: Your doctor will ask you about your symptoms and examine your body. He may perform tests and sometimes use imaging tests, such as an X-ray or an MRI.
- Medication: Analgesics, anti-inflammatory drugs, and muscle relaxants help relieve pain and inflammation.
- Physical Therapy: Specific exercises and stretches to improve flexibility, strengthen muscles, and reduce pressure on the sciatic nerve.
- Lifestyle Changes: Simple posture changes, avoidance of prolonged sitting, and regular exercise are helpful in long-term treatment.
- Injections: Injections can be used in more severe cases to reduce inflammation and temporarily relieve symptoms.
- Surgical Treatment: Surgical treatment is reserved when conservative measures have failed and is intended to address the underlying structural problem.
Why Professional Advice Is Important
Understanding sciatica is empowering, but seeking professional medical advice is critical. Self-diagnosis and treatment can lead to complications. Your doctor will provide you with personalized advice based on your specific situation and ensure the most effective course of action.
In summary, sciatica is like a warning signal from your body indicating a problem in your lower back. Understanding the different types allows individuals and medical professionals to work together to develop customized relief strategies. Knowledge can be your powerful ally in treating sciatica and guide you to informed decisions for a healthier, pain-free life.
Frequently Asked Questions
Q1: How can I determine the severity of my sciatica pain?
The severity of sciatica pain can be assessed based on the intensity, frequency, and duration of symptoms. If you experience persistent, sharp, or debilitating pain that interferes with your daily activities, it’s considered severe. Consulting with a healthcare professional can help determine the extent of your condition.
Q2: What are the signs of severe sciatica?
Signs of severe sciatica include intense, constant pain radiating down the leg, significant muscle weakness, numbness, or tingling. If you have difficulty walking or experience changes in bladder or bowel function, it’s crucial to seek immediate medical attention.
Q3: Is sciatica always severe, or can it be mild?
Sciatica can vary in severity. While some individuals may experience mild, occasional discomfort, others may experience moderate to severe pain. The severity depends on factors such as the underlying cause, the degree of nerve compression, and individual health.
Q4: What are the first-line treatments for managing sciatica at home?
Initial home care for sciatica may include rest, applying ice or heat, and over-the-counter pain medications. Gentle exercises and maintaining good posture can also help alleviate symptoms.
Q5: When is medical intervention necessary for sciatica?
Medical intervention is recommended when sciatica pain is persistent, severe, or accompanied by neurological symptoms. A healthcare professional may prescribe medications, recommend physical therapy, or consider more advanced interventions based on the severity of the condition.
Q6: What role does physical therapy play in treating sciatica?
Physical therapy is often a key component of sciatica treatment. Therapeutic exercises, stretching, and targeted interventions can help improve flexibility, strengthen muscles, and reduce pressure on the sciatic nerve.
Q7: Are there surgical options for treating stage 4 severe sciatica?
In cases of severe or persistent sciatica that doesn’t respond to conservative treatments, surgery may be considered. Surgical options may include discectomy, laminectomy, or other procedures aimed at relieving pressure on the affected nerve.
Q8: How can I prevent the recurrence of sciatica symptoms?
Preventing sciatica recurrence involves maintaining a healthy lifestyle, including regular exercise, proper lifting techniques, and good posture. Managing underlying conditions, such as obesity and practicing spine-friendly habits can contribute to long-term well-being.